How soon after exposure is Lead detectable in my child’s blood? What is the “half-life” of Lead in the bloodstream? How long does Lead stay in the body?
For those new to the Lead Safe Mama website:
Tamara Rubin is a multiple-federal-award-winning independent advocate for childhood Lead poisoning prevention and consumer goods safety, and a documentary filmmaker. She is also a mother of Lead-poisoned children (two of her four sons were acutely Lead-poisoned in 2005).
- Tamara owns and runs Lead Safe Mama, LLC — a unique community collaborative woman-owned small business for childhood Lead poisoning prevention and consumer goods safety.
- Since July 2022, the work of Lead Safe Mama, LLC has been responsible for six product recalls (FDA and CPSC).
- All test results reported on this website are science-based, accurate, and replicable.
- Please check out our press page to see some of the news coverage of our work, linked here.
Here’s a link from the CDC with some info on this topic.
A quote from the above-linked article: “Lead is cleared from the blood and soft tissues with a half-life of 1 to 2 months and more slowly from the skeleton, with a half-life of years to decades.”
#1.) How soon after exposure is Lead detectable in my child’s blood?
Lead is detectable in the blood immediately upon exposure in most cases. Lead “bio-mimics” Calcium — because Lead is “misidentified” as Calcium-like by certain metabolic processes. So, much the same way your body begins to process dietary Calcium the moment it enters your digestive system via your mouth, the body immediately begins to try to “utilize” Lead (with both inhalation and ingestion pathways) by substituting it for Calcium and storing it in place of Calcium in the body — in the brain, organs, and bones. This is the pathway by which Lead causes damage to normally Calcium-dense structures – like the tissues of the brain, bones, teeth, and organs. When the body substitutes Lead for structurally & neurologically/electrically critical Calcium, the body cannot function properly.
In my experience, many pediatricians and poison control center representatives are not up on the current science that demonstrates that Lead shows up in the blood immediately. I saw this (again) firsthand at the beginning of the CoviD Pandemic (early 2020)… A mama contacted me because her baby had swallowed some Lead pellets from inside a maraca. Poison control told her “not to worry!” I told her to rush to the Emergency Room and get an immediate Blood Lead Level (BLL) test. ER docs were also reluctant to administer the BLL test, but did so — and within a few hours of her child swallowing the pellets his BLL was registering 7.0 (µg/dL).
In conclusion: If you suspect an acute exposure, it is never “too soon” to get tested. It is also good to get tested right away because you want to be able to estimate what the highest exposure level was, so you can have a sense of the likely scope of possible impacts. Following an acute exposure, Blood Lead levels will start going down fairly quickly, too (if the source of exposure has been fully removed) and — while it is impossible to determine with certainty precisely what the peak levels might have been — if you don’t test right away, you may never know anything meaningful at all about the approximate highest BLL resulting from a specific event of acute exposure.
#2.) What is the “half-life” of Lead in blood?
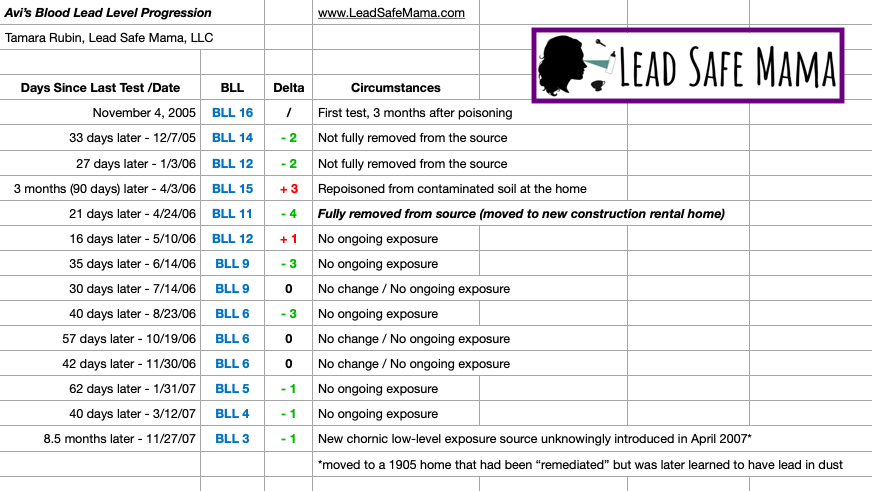
The chart below is the progression of my son Avi’s Blood Lead Level
over the two years after he was poisoned. Continue reading below the chart.
My children were acutely poisoned in early August, 2005. Avi was not tested until November 4, 2005 (about three months after his exposure), so we will likely never know how high his BLL was initially — but based on the scientific understanding of the half-life of Lead in the blood (which is a theory that does not often play out in practical real-world applications), we can guess…
The theoretical “half-life” of Lead in the blood (following an acute exposure) is understood by the medical community to be 30 to 45 days. Again, this is a theoretical construct — as one can only normally demonstrate this if the source of exposure is:
- Known and specific (clearly-identified and likely incident related)
- Subsequently completely/ fully removed
(Meeting both of these conditions is not always possible.)
In the case above of the little boy who swallowed the maraca pellets (a specific-event acute exposure), the source was both specifically known and removed fully. In the case of a child who is living in a Lead-painted house without remediation, identifying all primary exposure sources (especially for chronic/ persistent low level exposure) is less clear-cut, and thus knowing if the source of exposure has been fully removed (without constant thorough testing of both the home and the child) can also be more challenging.
Theory vs. Reality of Lower Levels
In practice (vs. theory), when children’s Blood Lead Levels get below a BLL 5.0, it seems that the remaining BLL points tend to come down more slowly (much more slowly than being reduced by half every 30 to 45 days) even if the source of exposure is fully removed. You can see a clear example of this when looking at the progression of my son Avi’s Blood Lead Levels from November 2005 through March 2007 on the chart above. It took nearly seven months (from August 23 to March 12th the following year) for Avi’s BLL to reduce from a BLL of 6.0 to a BLL of 4.0 even though he was fully removed from the source of his exposure during that period of time (we had moved to a new construction townhome in April of 2006 and did not move again until April 2007).
Given my sons’ initial exposure was a specific-event acute exposure (it occurred over just a couple of days), so we know the pathway of exposure (inhalation of Lead-containing fumes caused by the burning of Lead paint) AND the approximate date for the onset of severe/ acute symptomatic expression of their exposure (in retrospect, we know this because they became instantly quite sick when the workmen began torch burning the paint in early August, 2005), one might theoretically extrapolate the following:
- Tested 11/4/2005: BLL 16.0
- 30 days earlier (10/5/2005), likely/possibly in the neighborhood of BLL 32.0
- 30 days earlier (9/5/2005), likely/possibly in the neighborhood of BLL 64.0
- Initial poisoning in early August 2005, possible approximate BLL at initial exposure: 128.0
So while we cannot know for sure that Avi’s BLL was in fact initially a 128, it makes sense as a hypothetical extrapolation given observed typical “half-life” trajectories, as well as both the acute incidental nature of his exposure and the extreme/ dramatic symptoms he experienced from the moment (we later determined) he had been poisoned and in the months following his poisoning.
For an alternate scenario, let’s discuss a baby with a hypothetical BLL of 7.0:
In theory, the following progression might be expected if the child is removed fully from the source:
- Date of testing: 7.0
- 30 days later (theoretical minimum half-life): Baby might be down to a 3.5
- 30 days later: Baby might be down to a 1.75
- 30 days later: Baby might be down to a 0.875 (or “less than 1 microgram of Lead per deciliter of blood).
This is why, when a parent comes to me excited that their baby has dropped from a BLL of 7.0 to a BLL of (for example) 3.0 six months after the initial testing, I have concerns that there is possibly still a persistent chronic low-level exposure source impacting that kiddo (or that their low level BLL now is a “remainder” from a previously higher level — yet not known/ tested for — exposure at a younger age).
Separating “theory” from practical reality
Again, looking at the progression of my own children’s BLL’s, the half-life theory does not always play out. In my experience working with families, a failure of the half-life theory is especially likely to be observed when there has been a higher-level acute exposure in a very young, rapidly-growing baby (with consequent high cellular turnover), which can result in Lead levels fluctuating and not reducing quickly (even with complete removal of the child from a known source) — as relatively high amounts of Lead absorbed with an initial acute exposure may be released back into the bloodstream from tissues, organs, and bones as the child grows.
It is also for this reason (the possible potential for Lead that has been stored in their body to be released and recirculated) that non-medically supervised chelation (including food-based chelation and other non-medical interventions) is quite controversial.
#3.) How long does Lead stay in the body?
Well, Dr. Lanphear said it best in my film: “Ninety percent of the Lead that you have ever been exposed to is likely still in your body.” The half-life of Lead in tissue and bones is much longer than that of Lead in the bloodstream and the main mechanism through which a Blood Lead Level gradually comes down is that — rather than being eliminated — the Lead in the bloodstream is actually absorbed by the tissue, organs, and bones in the place of Calcium over time… so in most cases, when a child’s Blood Lead Level goes down, that does not mean the Lead has left their body. Lead continues to accumulate in tissue and bones throughout your lifetime with every exposure to any amount of Lead you encounter in your environment and then is sometimes released back into the bloodstream with high cellular turnover events (like pregnancy, menopause, and traumatic physical injury such as a bone fracture).
It is for this reason that primary prevention of childhood Lead-poisoning is key. This is also the reason we do ourselves a disservice if we do not at least try to eliminate all possible sources of bioavailable Lead from our lives — Leaded dishes, toys, old Lead-painted doors, windows, siding, or other architectural components; stained glass, Leaded crystal, Leaded brass, old solders, and Leaded sports equipment (like Leaded bullets or fishing weights, even uncoated Lead diving weights, etc.) — with widely-available, affordable, safer alternatives. There is no reason to have these items in our lives, and the more Lead-exposure sources we can remove, the healthier we will be long-term.
As always, thank you for reading and sharing Lead Safe Mama’s articles. You sharing this work keeps us doing what we do. Please let me know if you have any follow-up questions and I will do my best to answer them personally as soon as I have a moment.
Tamara Rubin
#LeadSafeMama
Never Miss an Important Article Again!
Join our Email List





Your work is so amazing. I pray that child will be ok. I have a question regarding old Christmas ornaments from maybe 40 years, glass, shaped bells and round balls, etc. My gut feeling is that color coating is full of lead. I am rethinking of keeping these old things around. I am much more aware of every item I pick up because of your amazing work. Another one just he other day, colored metal stylus for a smart phone. Mine I notice the color is rubbing off. I thought of buying a lead test swab to just check. Do you have any insights? My gut reaction it’s positive. It just seems everywhere. Thank you.
Hi Mary – the Christmas ornaments are likely leaded, the stylus is likely not leaded. It is unlikely that either of those would test positive using a home test kit – because the home test kits are really designed to test house paint – so it’s not worth spending the money. With vintage Christmas ornaments you have to evaluate if kids are going to touch and fidget with and hold them and how much interaction they will have. With the glass balls I figure that the biggest hazard is if they break and you are going to clean them up really thoroughly if they break anyway – so I am not concerned about potential hazards (since one is unlikely to let a small child play with them.) I have a greater concern for the little toy soldiers and other ornaments that look more like toys and that children are more likely to interact with like a toy.
Thank you for your kind words!
Tamara
Were you and your husband present in the house when your children were poisoned? Was wondering if you had any effects as well.
Yes – discussed here: https://tamararubin.com/2019/07/today-is-my-youngest-sons-11th-birthday-happy-birthday-charlie-parker-eliezer-rubin-the-story-of-how-lead-impacted-his-birth/
Tamara
We live in an old home that once had lead paint. (I know this, because there was an add on. The original exterior wall can been seen in the attic, and there is lead paint up there that is in very bad shape.) We never let our daughter play in the dirt, which has always felt strange. Well, today we were busy doing yard work, and our daughter started playing in the dirt by the house. The damage was done. The dirt was everywhere, and she said she got it in her mouth a few times. I haven’t tested the dirt, but we do have a lead test. I decided to do something strange. I took a paper towel and rubbed it in the dirt, and I used the lead test on it. It turned red, which is shocking. She’s had some exposure now, and I just feel like a terrible parent that our child was able to play with leaded dirt. (We test her once a year, and it always comes back below 1.) She’s five, so she can communicate very well. She said it wasn’t a lot. It essentially blew into her mouth from what it sounds, and it was crunchy, which we’ve all experienced at some point. This was just highly leaded dirt, which has me worried. We’ll get her tested and hope for the best.
Hi Tamara,
If a 9 month old had a BLL of 4.0 from a blood draw in January and three months later it was 3.9 also from a blood draw, from your experiences do you think this is consistent with chronic low level exposure or just slowly coming down? Thank you for the work you do. It is tough getting answers from the doctor. I’m assuming they just really don’t know much about lead exposure.
Those numbers are the same. Those number represent persistent / ongoing exposure. Have you watched my film yet? If not, here’s the link:
https://tamararubin.com/2023/01/a-link-to-my-film/
Tamara
Hi Tamara, we were living in an old house when our baby was born July 1, 2022. We left the house November 15, when he was 4.5 months. Came back for one week in late December, one week in late January, and one week in late February (by this time he was crawling). We discovered that there was lead paint on the windows and likely lead dust in the house. We had him tested in early April, at 9 months, and his lead level came back at 2.2. This was 6 weeks after his last visit to the house at the end of February. I’m wondering if this means he had chronic low exposure throughout his first 4.5 months from inhaling lead dust, or more acute exposure in late February once he was crawling/hands in mouth, etc. and ingesting lead dust from the floors. Trying to extrapolate to his highest level, and overall concerned about harm we could have caused our sweet baby unknowingly in his earliest months. Would sincerely appreciate your advice.
Hi – it could be either scenario. Have you watched my film yet? If not I encourage you to watch the film as it is a crash course for folks in your situation. Here’s the link: https://tamararubin.com/2023/01/a-link-to-my-film/
also please read this:
https://tamararubin.com/2017/01/toxic_lead/
And this (for context if not directly applicable to your situation):
https://tamararubin.com/2017/01/if-a-doctor-says-your-babys-blood-lead-level-is-normal-get-a-new-doctor-theres-no-normal-level-of-lead-in-blood/
Also this:
https://tamararubin.com/2023/03/ive-been-helping-a-mama-whose-doctor-had-unknowingly-put-her-on-a-high-lead-diet-that-poisoned-both-her-her-breast-fed-baby/
It’s hard to evaluate this from just a comment, but I do also do zoom consults to help families – here’s a link with more info on that.
https://tamararubin.com/2020/07/yes-i-do-phone-consultations-and-video-conferences-and-video-speaking-engagements/
In any case, start by watching the film.
Tamara
Hi! Is it possible for lead levels to decrease by over half in a matter of weeks? About 2.5 weeks ago, I had my 2 year old’s lead level tested as part of a routine checkup. I was surprised that it came back elevated at 8.6. The only thing I can think of is that a few months ago, I repaired some paint that was chipping off the wall near the window in his room, and must have exposed him with dust. My house was built in the 50’s. I washed the walls and floors with a lead cleaning solution, threw out and replaced his blinds and curtains, and washed the sheets, repainted the room with a lead encapsulate paint. My pediatrician wanted me to retest him to make sure it wasn’t a lab error and so I took him yesterday, and his levels were 4.1. We were also away for a week on vacation so I’m not sure what to think, or how it’s possible the level could drop by half in a matter of weeks. Also what would be an ideal timeframe to test him again to be sure that there is no residual lead dust in the house?
Hi Tamara,
So lead will substitute calcium in your body? I had testing done and found out that I was insufficient in calcium which was weird to me because I was consuming raw milk and dairy products. I recently was tested for heavy metals and came back high in lead. My level is 16. Would this explain why my calcium was insufficient?
Than you so much for your all your time and help! God bless you Tamara!