A Comprehensive Plan for Childhood Lead Poisoning Prevention Initiatitves: 2025-2028
As shared on Instagram
November 15, 2024
Last Updated: November 16, 2024
DRAFT IN-PROGRESS:
Here’s a list for Lead Poisoning Prevention Initiatives that could be implemented in the next four years (with a little collaboration, conversation, and enforcement)!
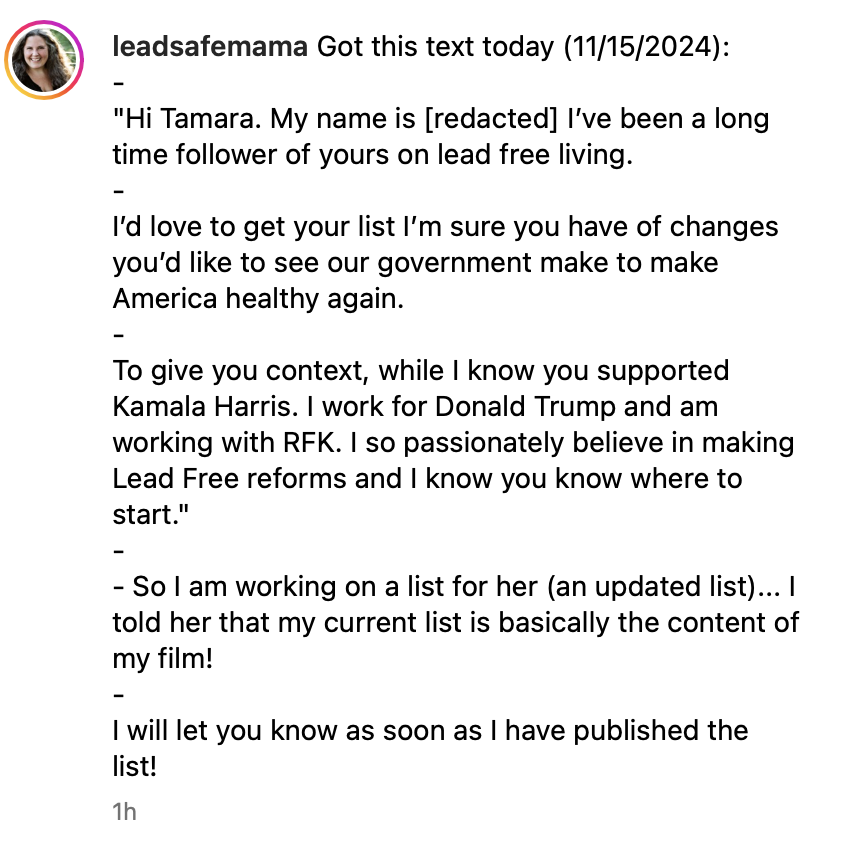
I will be working on this over the next couple of days (in response to the inquiry shared in the screenshot above)… It’s a draft outline right now, so check back here later. I will share it on the Lead Safe Mama email newsletter as soon as it is finished!
Background on the Issue of Childhood Lead Poisoning
- Childhood Lead poisoning is the single most societally expensive and single most preventable environmental illness impacting children (and families today).
- In 2011, Dr. Leonardo Trasande (currrently with NYU Medical) estimated (in his published environment impact report) that the total cost of environmental impacts on children’s health was $76,600,000,000 ($76.6 billion) annually.
- Of that $76.6 billion in annual impacts from toxic exposures to children, $50.9 billion of those costs were attributable to Lead exposure.
- Said another way, the environmental impacts of all toxicants combined — excluding Lead — is $25.7 billion annually.
- Said again another way, the impacts of all other chemicals combined on children’s health (mercury, bpa, pfas, plastics, etc.) is only about HALF the financial impacts of Lead alone.
- Lead poisoning was not eradicated with the 1978 “ban” on Lead in house paint, and is very much still a significant problem in the United States today.
- This $50.9 billion annual cost (in 2011) is conservative and focuses on medical impacts and I.Q. loss, both of which are metrics that do not begin to quantify the true financial impacts of Lead exposure. Costs omitted from this economic impact report include: Relocation costs, renovation funds, the lost income of parents managing their children’s Lead exposure and subsequent disabilities, legal system costs, long-term disability support costs, special education costs (through college and beyond), incarceration costs, and more.
- The true cost is much, much greater — likely in the range of hundreds of billions annually, in the United States alone — when every cost (both long-term and short-term) to families and society at-large is taken into account.
To reiterate: Childhood Lead Poisoning is the SINGLE MOST EXPENSIVE and SINGLE MOST PREVENTABLE environmental illness impacting families today. To not address this issue with a comprehensive plan for primary prevention would be criminal.
The guiding principle for each of these areas will be to rely on the latest science, which is not protective of industry but focused on fully protecting human health (with the priority being on protecting children, our most vulnerable citizens).
Focus Area Index (details for each of these areas are below)
- Maternal Health (Prenatal/ Preconception)
- Children’s Health (Birth to 18 years+)
- Comprehensive Blood Lead Level Testing (not age restricted)
- Occupational Health Standards and the Impact on Children
- Comprehensive Health Protective Standards for Lead in Housing
- Comprehensive Health Protective Standards for Lead in Water
- Comprehensive Protections for Children and Students in School (through college)
- Comprehensive Standardized Limits for Lead (and other toxicants) in all foods
- Comprehensive Regulation for Non-Food Personal Care Products
- Comprhensive Regulation of Cookware and Kitchenware
- Comprehensive Regulation of Decorative Consumer Goods
- Supporting Families of Lead-Poisoned Children
- Enforcement of Fine and Penalties to Landlords and Contractors
- Appointing an Appropriate XRF Instrument in Every Health Department
- Functional Disability Accommodations for People with Lead Poisoning in School
- Rights to Lead-free On-Campus Housing (especially when required)
- Comprehensive Education of Medical Providers
- Hazard Assessment of All Homes with Transfer of Resident (rental or purchase)
- Science-Based Improvements to the EPA’s RRP Rule
- Standards for Community Gardens
- Labeling Standards for Antique or Vintage Resale (ebay, etc.) Items (especially food-use products)
Focus Area #1)
Maternal Health (Preconception/ Prenatal)
Narrative: Childhood Lead poisoning prevention starts with mom. If mothers (and prospective mothers) are made aware of the persistent/ current/ ongoing concern for childhood Lead poisoning in America today, they will be in position to take action for primary prevention (preventing childhood Lead poisoning BEFORE it happens). Key actions include:
- All interventions below should not be contingent on any demographic factors (race, socio-economic, religion, etc.)
- Modeled after the Finnish baby box policy, which is for all citizens who have babies.
- Given the demonstrated impact of dietary concerns to elevate BLL’s above 0.5, traditional “risk factors” should not be considered (as they are no longer relevant).
- Comprehensive annual preconception blood Lead level (BLL*) testing (with the Pap Smear schedule), starting in the teen years.
- Comprehensive prenatal blood Lead level (BLL) testing, testing starting with the first OBGYN visit in pregnancy.
- Comprehensive public health education for women of childbearing age (starting in high school?) regarding Lead exposure and the potential impacts of Lead exposure on a child. This could be a one-day eight-hour class or a certificate class along the lines of current programs for “First Aid,” “CPR,” or “Pool Safety.”
- Interventions for women who test positive with a BLL of 0.3* (micrograms of Lead per deciliter of blood) or higher (with the above initiatives) include:
- Home assessments
- Dietary assessments
- Additional education
*0.3 is not arbitrary — it is based on Dr. Felicia Rabito’s research, a Tulane professor whose 2014 published study demonstrated that negative birth outcomes (and pregnancy complications) were correlated with BLL’s as low as 0.43 (and possibly lower).
BLL testing with point-of-care screening tools (in clinic) can cost as little as $7 per test (according to 2015 numbers). Magellan Diagnostic’s LeadCare II has just recently been approved for testing down to a BLL of 1.5. Labcorp can test down to BLL’s as low as 0.1 with a doctor’s prescription.
Focus Area #2)
Children’s Health (Birth to 18+ years)
Current standards and initiatives for childhood Lead poisoning prevention focus on children ages 1-year-old to six-years-old. This is a misguided focus as children of any age can be poisoned and children of any age (into young adulthood and beyond) can be greatly impacted by Lead exposure. Our responsibility to protect children from Lead exposure (and inform and educate parents) should start at birth and extend through college.
- Change recommended blood testing intervals to be more protective of children’s health.
- Pre-crawling (6 to 8 monhts)
- Post-crawling (12-15 months)
- Every 6 months through age 3
- Annually after age three, through age 18 (with annual checkups)
- Increase education to pediatricians regarding potential sources of Lead exposure that impact children of all ages
- Parental occupational exposures
- Dietary exposures
- Housing exposures
- School exposures
- Hobby related exposures for children (including hunting and shooting sports, fishing, model-making, electronic-focused hobbies, stained glass, etc.)
- Expand the pediatric screening questionnaire for childhood Lead poisoning to include the above considerations
- Remove socioeconomic considerations from the questionnaire
- Remove racial demographic from the questionnaire
- Support change to low threshold of detection for most commonly used BLL testing methodologies to lowest possible thresholds of detection (approaching 0.1 micrograms per decilitier)
Focus Area #3)
Blood Lead Testing (comprehensive, not age restricted)
Blood Lead Level Testing (BLL Testing) should be made available to all, covered by insurance without restrictions based on gender, age, or profession.
- Children should be tested through the teen years with their annual checkups
- Low threshold of detection should be standardized at 0.1 microgram of Lead per deciliter of blood
- Adult men should be tested to evaluate risk of heart disease and other related concerns
- Levels of detection for adult men should be the same used as those used for children with a low threshold of detection of 0.1 microgram of Lead per deciliter of blood
- OSHA standards that assert men are “safe” with an industrial exposure level of 20 (or 25) need to be changed across the board
- BLL 20 or 25 for an adult has never been health-protective, but has always only been protective of industry
- Men working on risky jobs that may have possible exposures from their occupation should be tested at least weekly and informed of the risk of persistent low level occupational exposure at the start of each job
- Adult women should not be told they are “ok” with a BLL under 5.0 (given levels as low as 0.43 have been demonstrated to cause harm). All standards (in medical training of doctors) referencing 5.0 as a safe BLL threshold of adult women need to be changed immediately.
- Women should get tested prior to conceiving
- Women should get tested upon conception and at the beginning of each trimester
- Seniors should get tested when they are at risk of bone density changes and in response to injury or accidents.
- Doctors should always test when stomach issues present without fever
- BLL testing should be added as a standard preventative measure at the beginning of each ER visit for a child (given some children only go to the doctor when it is the ER)
- This could be added along with the protocol for taking temperature and blood pressure
- This should be for children of all ages (through age 18 and later)
- ER doctors seeing children with stomach pain should automatically include a BLL test in the protocol (looking for BLL’s above 0.1)
- Activities that should trigger a standard BLL test for adults on their annual check up: Stained glass-making, hunting and shooting sports, fishing, occupational exposures, boating, furniture refinishing, model-making, antique collecting, etc.
Focus Area #4)
Occupational Health Standards (OSHA) and the Impact on Children
Children are often poisoned when their parents bring home Lead from work. As a result, OSHA standards need to extend beyond the immediate workplace exposure concerns to include the potential for a worker bringing hazards home to their families and exposing those family members to the occupational Lead they tracked home.
- OSHA standards for showering and changing clothes at the work place (for many professions, including house painting) need to be made mandatory.
- Workers with beards and long hair need education about the possibility of carrying Lead home to their babies via hair (many children have been poisoned this way, when baby hugs daddy and grabs his beard after work)
- Workers need to be educated about the possibility of carrying lead home in their cars. Workers need to be encouraged not to use their personal family cars (especially cars used to transport children) for Lead-related work.
- Protocols need to be put in place for periodic testing of workers personal spaces to ensure they are not bringing Lead home from work.
- There needs to be strict enforcement of handwashing before eating or smoking for any lead-related work (to limit Lead transferance from normal hand-to-mouth activity.
Focus Area #5)
Comprehensive Standards Protective of Children’s Health for Lead in Housing
The levels currently used for standards applied to housing (for water, soil, and house dust limits) are not protective of human health
- Dust wipe samples for Lead should be required before the transfer of residence into a pre-1978 home, or any age urban home.
- Dust wipe samples would need to test “non-detect” with a low threshold of detection of no more than 5 micrograms of Lead per square foot.
- Records of this testing should be kept on file with the city and accessible through a public records format, much like oil tank decommissioning and permit-related paperwork is kept on file for a property.
- A good template to use for this type of system is Portland, Oregon’s “PortlandMaps.com” program, where people can look up public information based on a property’s address.
- Water should be tested at the tap with transfer of residence and should follow the American Academy of Pediatrics recommendation that water consumed by children should not test positive above a threshold of 1 ppb Lead.
- The federal standard for Lead-in-Water should be lowered to 1 ppb Lead
- The standard for allowable Lead in schools (faucets, bubblers, sinks, etc.) should also not exceed 1 ppb Lead
- Dust wipe samples for buildings housing children should not be at-or-above 5 ppb in common areas (stairways, elevators, entrance areas, etc).
- These standards should apply regardless of whether-or-not a child lives in the building at the time of the testing.
- Soil should not test positive for levels above 40 ppb Lead, and if it does a family should be warned that the area is not safe for children.
- Soil levels below 40 ppb are common outside of urban areas.
- In urban areas, every effort should be made to remediate the soil and keep children away from contaminated soil.
Focus Area #6)
Comprehensive Standards Protective of Children’s Health for Lead in Water
The AAP has stated (for nearly a decade) that water consumed by children should not test positive for levels of Lead above 1 part per billion (ppb). This is the science-based level considered to be the most protective of human health. The FDA’s current standard for allowable limits of Lead in tap water is 15 ppb. The current allowable limit for Lead in bottled water is 5 ppb. Neither of these limits are acceptable, as children may drink water from any source. We need to work on monitoring the Lead levels anywhere a child may drink water, with a maximum allowable level of Lead being 1 ppb. These levels need to be monitored at least annually to confirm ongoing compliance. The records for monitoring water in public spaces (like schools, daycares, universities, or public water fountains) should be publicly available via an online, searchable/ accessible system.
- Lead levels in drinking water in homes (including bath water that children may also be expected to drink) should be monitored with the transfer of ownership or transfer of residence of a home to ensure compliance with a 1 ppb limit of Lead in water.
- Landlords should be required to test the water in residential and office units (at locations where water is used for drinking) annually, with records accessible and kept on file
- Schools should be required to monitor drinking water sources (including fountains) every three months (or more frequently depending on the requirements of any filtration system they used) at every source where a child or adult may be reasonably expected to drink water.
- This includes, as an example, a sink in a teacher’s lounge where the water is used to make coffee.
- Given that the presence of fluoride combined with chloramine in drinking water systems can increase the bioavailable Lead in the water between 800% and 1,100%, any water delivery systems currently treated with fluoride should have a full audit to determine the scope of concern (for a town, school, homes, etc.) and come up with a course of action in response to the levels found.
- In cases with this scenario that have resulted in elevated Lead levels in the water, cities and water districts will evaluate the possibility of removing fluoride from the water delivery system as a first step.
Focus Area #7)
Standardization of School Concerns (regardless of age of construction of school buildings) – for all schools, pre-K through University (including University Housing) – Water, Dust, Soil, Playgrounds (artificial turf)
- x
- x
- x
- x
Focus Area #8)
Standardization of Food Concerns (across all ingested products – Foods & Supplements)
- Babies eat all food, food should not be protected because it is baby food
- Harsh penalties for companies selling toxic products marketed and sold specifically for consumption by children
- x
- x
Focus Area #9)
Comprehensive Regulation for Non-Food Personal Care Products (toothpaste, cosmetics, face masks, baby powders, etc.)
- x
- x
- x
- x
Focus Area #10)
Comprhensive Regulation of Cookware and Kitchenware (all items used for preparation and serving of foods)
- x
- x
- x
- x
Focus Area #11)
Comprehensive Regulation of Decorative Consumer Goods (regardless of age of intended comsumer)
- x
- x
- x
- x
Focus Area #12)
Supporting Families of Lead Poisoned Children
Systemic racism in enforcement and compliance of DHHS/ CPS policies protecting children has continued to impact families of Lead-poisoned children in extremely harmful ways. Black families whose children are diagnosed with Lead poisoning are significantly more likely than white families to be threatened (by Child Protect Services or other agencies involved) with having their children removed from their home. In all cases, regardless or racial or socioeconomic factors, the separation of families with Lead-poisoned children should never happen. Instead, resources to support and relocate these families who are (in most cases) victims of negligent landlords should be allocated, and a structure of support should be put in place.
- Funding needs to be allocated to prioritize helping families in crisis when their children have been poisoned
- This funding should be modeled after the Bronx Montefiore Medical System’s program, which has a “safe house” program for families of children who have been Lead-poisoned.
- Families are given free, alternate, furnished, and safe (Lead-free) housing until their child’s medical situation has resolved.
- Families should be given appropriate medical treatment and interventions (alternate Lead-free housing is a medical intervention in the case of a Lead-poisoned child)
- This should be cost-free for impacted families.
- Regardless of the availability of an official “safe house” in an area, when a landlord is at fault (this includes any instance when a child has been poisoned in a rental home, in which the default conclusion should be that the landlord is “at fault”) the landlord should be made to pay immediate relocation costs for families (moving costs, plus first and last month’s rent, as well as the deposit for new, lead-free alternate housing).
- This housing needs to be appropriate and comparable for the family. For example, if the family has pets, the new alternate housing should also be pet-friendly and the landlord responsible for the child’s poisoning should pay any pet deposits as well.
- Landlords may push back against this policy, but the intention behind it is that NO children will be poisoned as landlords will be “encouraged” to remove all Lead hazards from their rental units so that children are NEVER poisoned. The responsibility of landlords to pay relocation costs will serve as a deterrent.
- Families should not be required to seek out sub-standard housing that is not equal to their current accommodations in amenities.
Focus Area #13)
Enforcement of Fine and Penalties to Landlords and Contractors
Focus area #14)
An appropriate XRF instrument in every health department, starting with each of the 52 State Health Departments (A 2025 version of A Chicken in Every Pot!)
Focus area #15)
Functional Disability Accommodations For People with Lead Poisoning in School (through college years and graduate school)
Focus area #16)
Right to Lead-free Required College Housing
Focus area #17)
Comprehensive Education of Medical Providers
Focus area #18)
Hazard Assessment of all Homes with Transfer of Resident (rental or purchase)
Focus area #19)
Science-Based Improvements to the EPA’s RRP Rule
Focus area #20)
Standards for Community Gardens
Community gardens are often developed as a solution to food scarcity in urban areas. Given the population being served by many community gardens is already an “at risk” community for Lead exposure concerns (living in a densely populated urban area), it is especially important that any community garden soil is confirmed clean (safe for growing produce) as part of the permitting process for such a garden.
- Community garden soil should not test positive for Lead at levels of 40 parts per million (ppm) or above
- Ideally, community garden soil should not test positive for Lead at 20 ppm and above
- Soil being provided to (delivered to) community gardens as top soil/ planting soil and should be tested before it can be sold and delivered (we need to have some regulation in the soil industry for this purpose).
- Community gardens should be required to pass testing of the soil before people can begin to plant in these gardens
- The cost for the testing of community garden soil should be covered by the local city or town, funded by federal grants (this will be a relatively minimal cost of done efficiently).
- This testing can be integrated into the permitting process for community garden.
- Community garden soil should be retested annually to confirm safety levels.
- Education should be provided to agencies and community groups creating community gardens about the risk of Lead exposure from contaminated soil in urban areas.
Focus area #21)
Labeling Standards for Resale of Vintage Antique Consumer Goods
Inculding reused housing components
- x
- x
- x
- x
What did I miss? 😉
For more information about the concern for childhood Lead poisoning, please watch the documentary film I directed and produced:
Never Miss an Important Article Again!
Join our Email List







WooHoo! And yay!!
After learning that RFKj was seeking input from the public for names of people who could join the Trump administration to bring much needed change to our country in the area of health, I went to his site to put your name in the hat. I didn’t know if you’d be down for a position, but your knowledge and experience would be a stellar addition. I am so glad someone “in the camp” knows your work and reached out to you. I’m sure this individual is the one who already nominated you, but others can vote to show their support and belief in you and your work.
What you’ve put together in response is proof that you would be a fantastic resource and addition.
https://discourse.nomineesforthepeople.com/t/tamara-rubin/4498
Thank you. Actually this is not who nominated me, another member of the Lead Safe Mama community nominated me. Thank you for sharing that link here.
Tamara
So you’re gonna be a sell out too?! Shame. But I’m not surprised!!
We have no choice. Trump was elected president. This is a fact. If there is an opportunity to help children under this new administration, we should take it (we should at least try to make it work).
T
There’s always a choice.
I think it’s pretty clear Tamara is choosing the children.
This is awesome!!! So wonderful that they are reaching out to you and that you are going to help them out! Your experience and knowledge about lead issues being used in government to actually make changes is a dream come true.
Excellent start! ❤
Unless I missed it, I’m not seeing leaded aviation fuel on this list. Children living or attending school near general aviation airports continue to be poisoned by lead in the air and soil. The EPA have been dragging their feet on this for decades now. It’s time to support the scientists who are working on unleaded alternatives and incentivize airports to minimize the use of leaded avgas as much as they can (with an eventual ban in the future).
Perhaps also funding for homeowners and landlords to help remove lead exposures from their properties?
And some kind of requirements for standardized handling of public lead hazards (like fire hydrant paint – this really both affects the public and the homeowner whose land the hydrant is on).
Also, like you, I am not a Trump supporter (I voted 3rd party), but if RFK will actually make improvements in environmental toxins, I think we should support these kind of specific initiatives.
Well, I never disliked any politician as much as I dislike Trump! (Censored ) But we are stuck with this administration for the next 4 years and I hope and pray that they open their eyes to the real problems in the United States and start doing something about them!
Hi Tamara
I am wondering if Focus Area 16 can be amended to the following:
Not just housing but all buildings on college campus should be toxin free. Anywhere students will be in contact with should be toxic free.
Reason:
https://www.usatoday.com/story/news/health/2024/04/02/north-carolina-state-poe-hall-cancer-cases/73177821007/
Maybe add a focus area for medical research on treatments for lead poisoning. Right now there is only chemical chelation. There has to be better treatment for children and adults as chelation has it own toxicity.
Thanks
Dust wipe samples can (and will) be gamed by sellers with thorough cleaning prior to an inspector visiting the property. Painted window sills, door frames, floors, door steps, stair rails, door handles and other areas of increased potential for wear and dust generation should be XRF tested. Similarly, water sample testing can be gamed by running the tap for a while before the test, but water sitting in the pipes for several hours (such as overnight) can build up unsafe levels of lead.
Yes – these points are discussed in my film.
Please mention strict food labeling. For companies insisting they are putting their best products on the market, I would like clear packaging material that tells me the heavy metal content of ingestible products like food and supplements.
Thank you for writing this. I look forward to having it to refer to when people ask what we should be doing about these widespread issues.